Latest from NHS England:
-
NHS approves new IT system for GPs to help transform care
Source: NHS England (Top Bar) Published on 2025-06-25
About Total Health Excellence PCNs
What are Primary Care Networks?
Primary care networks (PCNs). Bring groups of general practices together to work in collaboration for the better health of people in their communities, providing community and practice-based services and enabling people to stay out of hospital by caring for them in their own homes
Enabling Practices to work in groups as part of a Primary Care Network increases their ability to recruit and retain staff; to manage financial and estates pressures; to provide a wider range of services to patients and to more easily integrate with the wider health and care system.
While GP practices have been finding different ways of working together over many years – for example in super-partnerships, federations, clusters and networks – the NHS long-term plan and the five-year GP contract, published in January 2019, put a more formal structure around this way of working, but without creating new statutory bodies, by creating Primary Care Networks.
All except a handful of GP practices in England have come together in around 1,250 geographical networks covering populations of approximately 30–50,000 patients.
It is not compulsory for practices to join a network, but they risk losing out on significant extra funding if they do not, and their neighbouring networks will be funded to provide services to those patients whose practice is not covered by a network.
Serving a population of circa 79,000 people.
Across the PCN network
What do Primary Care Networks do?
Primary Care Networks are a key vehicle for delivering many of the commitments in the long-term health of the nation plan and providing a wider range of services to patients. They are providing services such as structured medication reviews, enhanced health care in care homes, supporting early cancer diagnosis and understanding local health needs in order to tackle local inequalities.
They work with their partners to provide a wider range of primary care services to patients, involving a wider set of staff roles than might be feasible in individual practices, for example, first contact physiotherapy, extended access and social prescribing.
Networks are also the footprint for deciding which integrated community-based teams will develop, and community and mental health services will be expected to configure their services around PCN boundaries. These teams will provide services to people with more complex needs, providing proactive and anticipatory care.
In East Kent we have 16 PCNs.
Our executive team
An executive member from each of the practices is also included on our board.
Our Practices
Our service area is divided into two areas – West (Covering Folkestone), and East (Covering Dover and Surrounding).
West PCN (Folkestone)
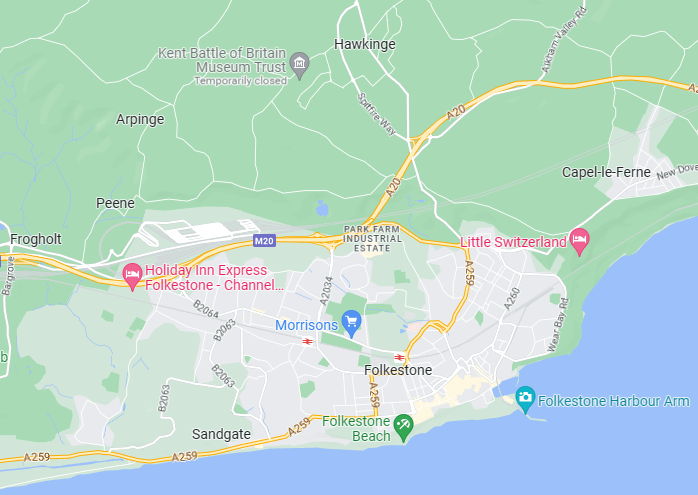
Guildhall St Surgery
Manor Clinic
Sandgate Road Surgery
The New Surgery
East PCN (Dover & Surrounding)
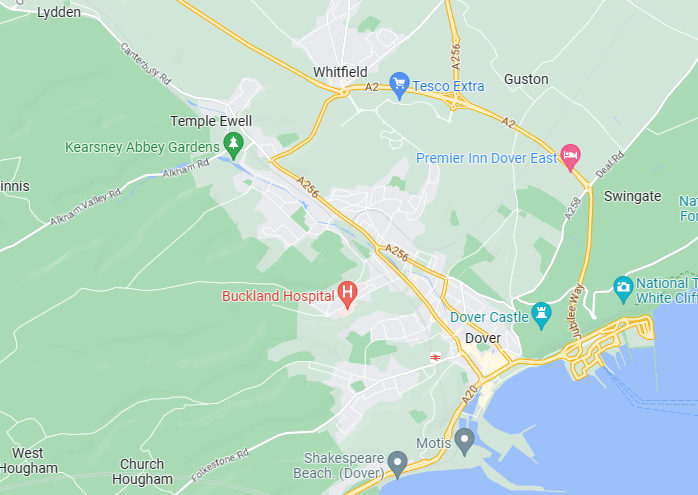
Lydden Surgery
Whitecliffs Medical Centre
Pencester Surgery
Aylesham Medical Practice